NanoKnife
Cancer of the prostate can vary from very small low-grade tumours that do not require treatment, to large high-grade cancers that present a threat to life and health.
These latter cancers require a major intervention to cure them.
This is most commonly total removal of the prostate called a Robotic Radical Prostatectomy.
There are in addition, however, a small group of prostate cancers that are small and localised, but that still require treatment.
These are amenable to focal therapy.
Focal therapy
Focal therapy is treatment of the part of the prostate containing the main or significant cancer, while leaving the rest of the prostate intact and unaffected.
Prostate cancer is usually multi-focal, i.e. there are usually several areas of cancer in the gland, but one area will be larger and of a higher grade of malignancy than the rest.
The aim is to eliminate this main or significant area of cancer, allowing the other areas to be monitored.
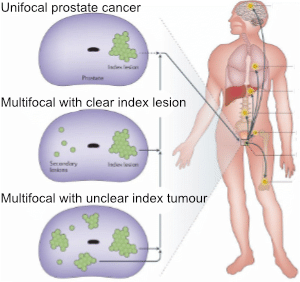
Figure 1 showing an index or significant cancer in the prostate
NanoKnife
NanoKnife, also known as Irreversible Electroporation (IRE) therapy is a form of focal treatment for cancer of the prostate.
There are a number of forms of focal therapy:
- High Intensity Focal Ultrasound (HIFU) which focuses ultrasound waves on parts of the prostate to heat these areas to kill the cancer cells.
- Focal Brachytherapy which places radioactive seeds into the area of the prostate containing the cancer.
- Photodynamic therapy (TOOKAD) in which a dye is injected and then activated with a laser to cause death of cancer cells.
- Cryotherapy where probes are placed into the prostate, and cooled to produce an ice ball which destroys the area of the prostate containing the cancer.
None of these therapies have been particularly successful, and can cause damage to surrounding structures such as the nerves, urethra and sphincter muscle.
Ideally therefore we want a treatment that only kills the cancer cells, but leaves the surrounding structures undamaged. This is achieved by the NanoKnife.
NanoKnife or Irreversible Electroporation (IRE) consists of placing a number of electrodes into the prostate to surround the area of significant cancer.
Short pulses of electricity using very high voltage are passed between the electrodes. This causes micropores to occur in all cells, including the cancer cells, which lead to their death.
This occurs by the process of apoptosis or natural (programmed) cell death. This does not cause inflammation which the other heat-based focal therapies do. Only cells are damaged.
Other structures such as the nerves, urethra and sphincter are unaffected, as they are not cells but supporting structures. Hence continence and erections are less likely to be affected.

Figure 2 The electrical field causes micropores to develop in the cell membrane which leads to cell death by Apoptosis. The dead cells are then removed by normal body mechanisms.
Once the needles have been placed in the prostate electrical pulses are delivered by the generator.
The voltage used, and the number of pulses and duration of the pulses are determined by the surgeon to ensure effective complete ablation or destruction of the desired area.

Figure 3: The generator, shown on the left, produces the high voltage and short pulses of electricity. The needle electrodes are placed around the area of cancer in the prostate.
The area of the prostate to treat is determined by an MRI of the prostate which can show the cancer in the prostate.
This is followed by a Trans Perineal Template Biopsy (TPTBx) of the prostate to confirm the presence and location of the cancer.

Figure 4: MRI showing the area of cancer at the back of the prostate on the patient’s left hand side. The prostate is seen as a cross section, with one standing at the feet looking at the patient’s head. The cancer shows as a dark spot on the T2 image (left photo), a dark area on the ADC map (centre photo) and as a white area on the DWI image (right photo).
A Prostate Specific Membrane Antigen PET scan (PSMA PET) may also be used to help define the area of cancer.
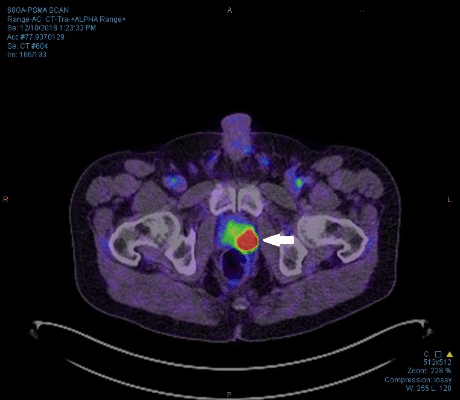
Figure 5: A PSMA PET scan showing the area of cancer in the patient’s left side of the prostate
The electrodes are placed by going through the perineum or crutch.
A transrectal ultrasound probe is used to visualise the prostate so as to ensure the accurate placement of the needle electrodes around the cancer.
This is the same technique that is used when carrying out a Trans Perineal Template Biopsy of the Prostate.
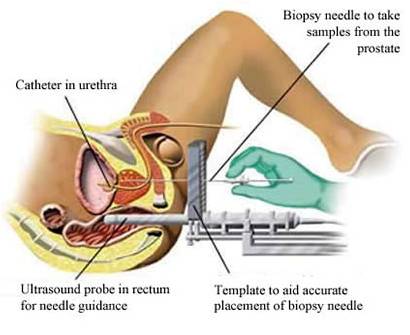
Figure 6: Trans-Perineal biopsy of the Prostate using a Brachytherapy grid to direct the biopsies.
The patient is in the lithotomy position, with the electrodes placed via the perineum using a Brachytherapy grid and Trans Rectal Ultrasound.
NanoKnife therapy is still in its early days as a treatment for cancer of the prostate, nevertheless, the results of studies to date show that with one or two treatments, 90% of men were rendered free of significant cancer, with less than 10% requiring a further intervention or therapy. Almost all men (98.8%) remained continent (i.e. free of the need to wear a pad), with the majority (90%) retaining their erections. (Blazevski, Stricker et al. USANZ ASM Poster April 2019).
It should not be considered as equivalent to Radical Prostatectomy or Radiotherapy, both of which are whole gland treatments designed to cure the cancer long term.
Ideally it should be considered as an alternative to Watchful Waiting for Prostate Cancer in older men.
It is best reserved for:
- Patients with smaller cancers of the prostate, where the lesion is clearly defined on the MRI and confirmed on the Trans Perineal biopsies.
- Low to moderate-grade cancers. These would be high-volume Gleason Score 6 (Grade Group 1), low Gleason score 7 (Grade Group 2) and high Gleason score 7 (Grade Group 3) cancers of the prostate. It is not appropriate for high-grade cancers of the prostate (Gleason score 8 and 9 or Grade Groups 4 and 5).
- Older men when treatment is desirable rather than Watchful Waiting, but when a full Radical Prostatectomy is either unsuitable or where the patient does not wish to have a radical treatment. Watchful Waiting is where there is a significant cancer present, but where its rate of progress may be slow. An older male may therefore choose to watch the cancer for a time, and asses its progress with serial PSA tests before deciding whether to actively treat the cancer or not.
Its main advantage is that it is a minimally invasive therapy that gives the patient a high probability of retaining their erections, with a very low risk of incontinence.
The procedure can be repeated if necessary. It does not preclude or make more difficult a Robotic Radical Prostatectomy if one is required at a later date. Similarly Radiotherapy can also be used later on if necessary.
It can also be used as salvage therapy in patients who have already had radiotherapy to their prostate cancer which has failed to clear the cancer. The NanoKnife therapy may then fully clear the cancer without making incontinence or impotence worse.
The procedure
Patients are admitted on the day of surgery. Blood thinning medication needs to be stopped prior to the procedure. The timing of when to stop will depend on which medication the patient is taking and the reason for taking it. A mild oral and suppository bowel preparation is necessary to ensure a clean bowel to allow the prostate to be clearly seen on the ultrasound.
The procedure is carried out under full general anaesthetic, and takes between 1 and 1 ½ hours. A catheter is left in the bladder at the end of the procedure, and this is left in for approximately five days. This is because the procedure may cause some difficulty in passing urine for a time. Patients would normally be discharged the following day. They then return to the rooms for a Trial of Void (TOV) where the practice nurse removes the catheter. Patients would then remain for a time to check that they are passing urine satisfactorily.
Patients then need careful follow-up to ensure the treatment has been successful. A PSA blood test will be measured at three, six and 12 months, and yearly thereafter. A follow-up MRI of the prostate will be done at 6 months, with a repeat Trans Perineal Biopsy of the prostate at 12 months.
The impact of the treatment on continence, erections and bowel function is assessed with regular questionnaires.
Currently it is expensive, as there is no Medicare item number for it, but it is available in the private sector at Epworth in Australia.
Disclaimer: The information on this website is provided for your general information and is not a substitute for the specific advice of your treating doctor.

