Transurethral Resection of Prostate (TURP)
- What is the prostate gland?
- What is a TURP?
- What are the benefits of TURP?
- What do I need to prepare before the operation?
- What happens after the operation?
- Will it hurt?
- The next day
- Catheter care and removal
- When you get home
- Top
What is the prostate gland?
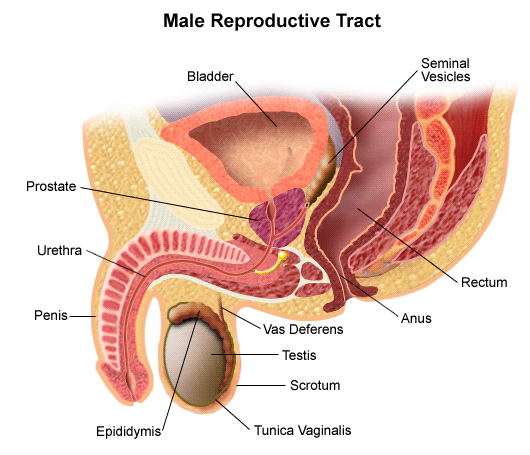
The prostate gland is only present in men. It sits below the bladder and surrounds the tube through which men pass urine (the urethra). When a man has an orgasm, the prostate gland produces most of the fluid, the semen, which nourishes the sperm.
What is a TURP?
It is an operation to create a larger channel through the prostate gland to prevent or relieve obstruction to the flow of urine. During the operation, a small telescope is passed through the urethra (wee pipe) and instruments are passed up the telescope to core out the inside of the prostate gland. There is no wound and no stitches are needed. The length of stay in hospital varies from 1-3 days depending on your recovery.
What are the benefits of TURP?
As men age, the prostate gland grows slowly. In some men it enlarges to cause a number of problems or symptoms, such as:
- Slow and poor urine stream
- Hesitancy (it may take a few seconds or occasionally up to a minute for the urine stream to start)
- Straining to urinate
- Feeling of incomplete bladder emptying
- Urgency (urgent need to go to the toilet without much warning)
- Frequency (going more than six times a day)
- Nocturia (going more than twice a night)
A TURP is most often done to relieve such symptoms. A small number of men develop complete blockage and suddenly find they cannot pass urine at all. This is called acute urinary retention. If this happens, it is usually necessary for a doctor to pass a fine tube (catheter) into the bladder to allow it to empty.
What do I need to prepare before the operation?
Tell your doctor if you are taking any medication including natural medicine and supplements e.g. vitamins or fish oil supplements.
If you regularly take drugs which thin the blood, such as aspirin, warfarin, Plavix, apixaban etc. please contact the Urology Nurse or your surgeon so they can advise you when to stop taking the medication before your operation.
When you arrive on the day of surgery, you will be asked to get ready for theatre probably quite soon after coming into hospital. This means changing into a theatre gown and putting on a pair of surgical stockings. These will help prevent a blood clot forming in the legs. We will do blood tests if you have not already had them. You must not have anything to eat or drink for at least six hours before the surgery, not even water.
What happens after the operation?
If you have had a general anaesthetic, you will wake up in the recovery room near the theatre. If you have a spinal anaesthetic, you will already be awake, but you will have a feeling of numbness from the waist down. This will last for a few hours post the surgery and is normal. You may also have some pins and needles when it is wearing off. A nurse will take your blood pressure and pulse regularly and will be available via the nurse call-bell system at any time. You will have a drip in your arm to give you the fluids you need. This is removed when you are drinking normally.
You will have a flexible tube (catheter) coming out of your penis. This drains the urine into a plastic bag at the side of your bed. Another tube will be attached to the catheter which will allow saline to flush your bladder. The catheter will be removed after 36-48 hours. The catheter acts as a flushing system. Do not be alarmed to see blood (coloured like red wine) in the catheter bag. This is normal. While the catheter is in place, you may get the urge to pass urine. This is quite normal, and you will realise that urine is flowing out of the bladder automatically along the catheter all the time, without any need to strain.
During the operation the prostate tissue has been scraped away, leaving a raw area that heals slowly over the next few weeks. While it is healing, the area will bleed.
Will it hurt?
Some people find the catheter uncomfortable, but most hardly notice it. Pain is unusual. If you have pain or discomfort, your nurse will give you some painkillers. During the first days a clot of blood may block the catheter. The bladder will become full and you will have an intense desire to pass water, but urine will be unable to drain out. If you think this has happened please tell the nurse. They can then flush the catheter with a syringe to clear it.
The next day
The doctor will generally visit at some time during the day to check your progress. You will probably be eating and drinking normally by now and the drip will be removed. You will be encouraged to drink about 1-2L of fluid each day to continue flushing the bladder. If the bleeding is settling down, the bladder flushing fluid will be stopped, but the catheter will stay in a day or two longer. If you have not already done so, you will be encouraged to get out of bed and start to walk around.
Catheter care and removal
Once the doctor is happy that the bleeding has settled down and you have had a bowel action, the catheter will be removed (usually the second day). After removal of the catheter it may take a while to control your urine flow immediately. You may feel a constant urge to urinate, have leakages or tend to dribble, or you may have difficulty urinating. Do not worry. These symptoms are all normal and will improve with time. You may experience some burning or stinging when urinating. This will settle down over the next few days.
When you get home
Tiredness: You should take things easy for about two weeks. Tiredness is very common and will last longer than you think, even up to a month after leaving hospital.
Bleeding: You will see blood or small clots in your urine, but this will slowly settle down over the next few weeks. This is normal after this surgery. It will be more noticeable some days compared to others, and in the morning when you have not drunk for a while. A little extra bleeding is common around the second week after the operation, as the scabs that have formed in the prostate come away.
Leakages on passing urine: You may find you leak a little when straining or coughing. This can be managed by wearing a small pad inside your underpants and is temporary. Frequent visits to the toilet and having to get up at night are also common and will slowly settle down. Many men worry about the possibility of incontinence after the operation. This is very rare and usually clears up, please talk to your doctor if you are concerned.
Exercise: Short walks are safe. Anything more active like jogging, digging and lifting should be totally avoided. Sports such as golf, cycling and swimming may be resumed after a month or so.
Diet: You can eat normally but try to ensure a high intake of fruit and vegetables, and other high-fibre foods to help avoid constipation. If you do become constipated, it is very important not to strain as this puts pressure on the healing wound. Try a mild laxative or ask your doctor or nurse for advice. Continue to drink 1.5-2 litres of fluid each day for the first week or two, to continue the flushing process and to help prevent infection. Increase fluids if you notice the urine becoming more bloodstained. Alcohol is permitted in moderation. Try to reduce drinking after 6-8pm so you do not have to get up during the night.
Driving: Do not drive for the first two weeks after the operation. This is because if you had to do an emergency stop, the sudden jerking movement could damage the healing wound.
Sex: You should not have sex for four weeks after the operation, as this may cause the internal wound to bleed.
Impotence: This isn’t usually a problem and some men find their erections improve. You may also experience retrograde ejaculation where semen passes into your bladder during orgasm instead of out of the penis. Retrograde ejaculation isn’t usually a problem, but it may reduce fertility.
Difficulty passing urine: Sometimes when the bladder muscles have been stretched or straining for a long time, it is necessary to rest them. A small proportion of men are unable to pass urine adequately afterwards and have to be sent home with their catheter in place for about a month. In this case we will give you full instructions on catheter care. You would then come back for a day visit to have the catheter removed and progress monitored for a few hours. Some men may learn to pass a catheter in and out on themselves.
Possible complications: The following symptoms may indicate an infection, which would need treatment from your doctor:
- A high temperature
- Continued pain, stinging or burning when you urinate
- Your urine comes back thick, cloudy or smelly
- Your testicles become swollen or painful
Heavy bleeding or blood clots may block the flow of urine and will become very painful. However, this is uncommon. If this occurs, please call your urologist or visit Epworth Richmond Emergency department at 89 Bridge Road (enter via Erin St).
About 1 in 10 men who have a TURP will need a further operation as the prostate tissue regrows. However, this may take several years to happen.
Follow up is generally 6-8 weeks after your operation. Please call your surgeon’s rooms if you do not have an appointment once you have been discharged.
Further information:
If you have any concerns or questions about your TURP, please contact as below:
- Urology Nurse: 03 8415 1915 (during business hours)
- Your surgeon
- Ward 1 East 03 9483 3602
Disclaimer: The information on this website is provided for your general information and is not a substitute for the specific advice of your treating doctor.

